You spend every day on your feet and put them through a lot. The foot is made up of 26 delicate bones, linking together with a network of tendons and muscles that connect to your ankle joints. With this many parts to the ankles and feet, there are many places where damage can occur.
Causes of a Broken ankle or foot
Broken bones are caused by an impact or sustained pressure that is more than the bone can take. Some common causes include:
- dropping something heavy on the foot
- hitting your toe against a piece of furniture or door frame
- sports injuries
- a severe twist or sprain
- falling from a height, especially onto a hard surface
Symptoms of a broken foot or ankle
At first it can be hard to tell the difference between a bad sprain and a broken bone. You should always visit a doctor if you suspect a break. Some symptoms include:
- sharp pain centered on the break or radiating through the foot
- swelling
- deep bruising
- a grinding sound or sensation when you move the foot
- physical deformation, especially for broken toes
- inability to walk on the foot
For this last point, keep in mind that broken toes may be less painful and you may be able to walk on them.
How are broken ankles and feet treated?
Your doctor will probably order an x-ray to determine exactly what happened and where the break is. For a broken ankle, a splint may be used. If it’s a severe break, you may need reconstructive surgery. In the case of broken bones in the foot, you may be given a cast, walking boot, or wheelchair to help you keep pressure off the area as it heals. For broken toes, the doctor will most likely splint one to an adjacent toe.





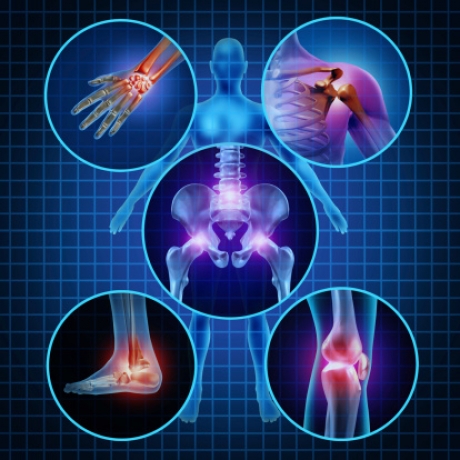
 Rotator cuff tendonitis occurs when the tendons and muscles that help move the shoulder joint are inflamed or irritated. This condition commonly occurs in people who play sports that frequently require extending the arm over the head, such as tennis, swimming and pitching. Most people with rotator cuff tendinitis can regain full function of the shoulder without any pain after treatment.
Rotator cuff tendonitis occurs when the tendons and muscles that help move the shoulder joint are inflamed or irritated. This condition commonly occurs in people who play sports that frequently require extending the arm over the head, such as tennis, swimming and pitching. Most people with rotator cuff tendinitis can regain full function of the shoulder without any pain after treatment.

