Osteoporosis is a disease that causes the skeleton to weaken and the bones to break. While most people think of osteoporosis as a woman’s disease, it poses a significant threat to millions of men in the United States.
There are many lifestyle habits that put men at increased risk of osteoporosis, yet few men recognize the disease as a significant threat to their mobility and independence.
Osteoporosis is called a “silent disease” because it progresses without symptoms until a fracture occurs. It develops less often in men than in women because men have larger skeletons, their bone loss starts later and progresses more slowly, and they have no period of rapid hormonal change and bone loss. However, in the past few years the problem of osteoporosis in men has become more recognized, particularly in light of estimates that the number of men above the age of 70 will continue to increase as life expectancy continues to rise.
Bone is constantly changing. Old bone is removed and replaced by new bone. During childhood, more bone is produced than removed, so the skeleton grows in both size and strength. For most people, bone mass peaks during the third decade of life. By this age, men typically have accumulated more bone mass than women. After this point, the amount of bone in the skeleton typically begins to decline slowly as removal of old bone exceeds formation of new bone.
Men in their fifties do not experience the rapid loss of bone mass that women do in the years following menopause. But by age 65 or 70, men and women are losing bone mass at the same rate, and the absorption of calcium, an essential nutrient for bone health throughout life, decreases in both sexes. Excessive bone loss causes bone to become fragile and more likely to fracture.
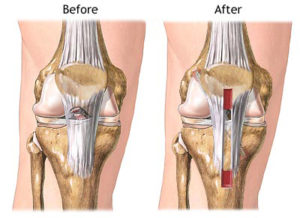
Fractures resulting from osteoporosis most commonly occur in the hip, spine, and wrist, and can be permanently disabling. Hip fractures are especially dangerous. Perhaps because such fractures tend to occur at older ages in men than in women, men who sustain hip fractures are more likely than women to die from complications.
In addition to age-related bone loss, there are many lifestyle behaviors, diseases and medications that can hasten bone loss in men. These include:
• Chronic diseases that affect the kidneys, lungs, stomach, and intestines, or alter hormone level
• Regular use of certain medications, such as glucocorticoids
• Undiagnosed low levels of the sex hormone testosterone
• Unhealthy lifestyle habits: smoking, excessive alcohol use, low calcium intake, and inadequate physical exercise
• Age. The older you are, the greater your risk
• Race. Caucasian men appear to be at particularly high risk, but all men can develop this disease.
Osteoporosis can be effectively treated if it is detected before significant bone loss has occurred. An orthopedic physician can order a medical workup to diagnose osteoporosis, including a complete medical history, x-rays, and urine and blood tests. The doctor may also order a bone mineral density test to determine your risk for fractures (broken bones), and measure your response to osteoporosis treatment.
In men, osteoporosis is often not diagnosed until a fracture occurs or a man complains of back pain and sees his doctor. This makes it especially important for men to inform their doctors about risk factors for developing osteoporosis, loss of height or change in posture, a fracture, or sudden back pain.
Once a man has been diagnosed with osteoporosis, his orthopedic physician may prescribe medications as well as a treatment plan including nutrition, exercise, and lifestyle guidelines for preventing bone loss.
Other possible prevention or treatment approaches include calcium and/or vitamin D supplements and regular physical activity.
Experts agree that both men and women should take the following steps to preserve their bone health:
• Avoid smoking, reduce alcohol intake, and increase physical activity
• Ensure a daily calcium intake that is adequate for your age
• Ensure an adequate intake of vitamin D
• Engage in a regular regimen of weight-bearing exercises in which bones and muscles work against gravity. This might include walking, jogging, racquet sports, climbing stairs, team sports, weight training, and using resistance machines
• Discuss with your doctor the use of medications that are known to cause bone loss, such as glucocorticoids
• Recognize and seek treatment for any underlying medical conditions that affect bone health