At this time of year, many individual can’t wait to leap into spring, getting back to the gym to drop some winter weight, or onto the golf course or other playing field. Proceed with caution! Sports injuries can be caused by poor training practices, improper gear and not warming up or stretching enough. People often get hurt because they are not in shape and take on too much, too soon.
The most common sports injuries are:
- Achilles tendon injuries
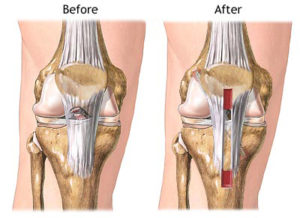
- ACL tears
- Dislocations
- Fractures
- Knee injuries
- Pain along the shin bone
- Rotator cuff injuries
- Sprains and strains
- Stress fractures
- Swollen muscles
- Tennis elbow
If you do get injured, stop. Continuing to play or exercise can cause more harm. Treatment often begins with the RICE (Rest, Ice, Compression, and Elevation) method to relieve pain, reduce swelling, and speed healing. Other possible treatments include pain relievers, keeping the injured area from moving, rehabilitation, and sometimes surgery.
It’s important to know when to look further than your medicine cabinet to treat sports injuries. An orthopedic surgeon is a medical doctor or doctor of osteopathy with extensive training in keeping your bones, joints, ligaments, muscles, tendons, cartilage and spine in good working order. Together, all of these parts of our bodies make up our musculoskeletal system.
Orthopaedic surgeons have the greatest knowledge of and experience with the wide range of conditions and treatment options available in musculoskeletal care, many of which do not involve surgery. However, if surgery is the best option for recovery, an orthopedic surgeon is the best trained to provide that surgical treatment.
Orthopaedic surgeons use the most effective and efficient diagnostic tools and our experience in musculoskeletal treatment to determine the best care for our patients.
Initial treatment of an injury following the basic RICE formula may be all you need, but if your injury does not heal on its own and continues to be painful, swollen or stiff, you may need surgery.
Depending upon the type of injury, your age and other factors, your orthopedic surgeon may recommend minimally invasive surgery such as arthroscopy following by physical therapy to help you resume your normal activities. In other cases, more traditional surgical repair may be recommended by your orthopedic surgeon.
Sometimes preventing common sports injuries is beyond our control, but many times sports injuries are preventable. Working out regularly will help you to enjoy your sports activities safely and you’ll garner extra health benefits as well. If you feel your sports injury isn’t healing on its own, consult an experienced orthopedic surgeon to help you get well and back into the game as soon as possible.