Many people seeking the best orthopedic surgeons near me in Monmouth County find Dr. Marshall P. Allegra. Dr. Marshall P. Allegra is a board-certified orthopedic surgeon in medical practice in Monmouth County for over two decades. He is a member of the American Academy of Orthopedic Surgeons and a Diplomate of the American Board of Orthopedic Surgeons.
Finding an Orthopedic Surgeon near me
Dr. Marshall P. Allegra specializes in full and partial joint reconstruction, arthroscopic surgery, hand, foot and ankle surgery and offers non-surgical care for fractures. When you visit his practice, he’s the only doctor you’ll see. He is patient-focused and an excellent diagnostician. He will determine the root cause of your pain and determine the best treatment options. Dr. Allegra has helped more than 500 patients with knee and hip replacements from Monmouth County and other surrounding areas.
About Orthopedic Surgeon Dr. Marshall P. Allegra
Turn to Dr. Marshall P. Allegra for all of your hand, wrist, foot and ankle surgeries. He is trained and experienced in the reconstruction of bones, muscles and tendons in the hands, feet and ankles. Using the latest in medical technology, he has successfully treated athletic injuries, tumors, carpal tunnel syndrome and more. His goal is to restore you to a pain-free active life. We use our hands and feet for everyday tasks and activities. It’s not uncommon to incur an injury due to accident or overuse. Contact Dr. Marshall P. Allegra for a one-on-one consultation. He’ll let you know what your treatments are, so you can get back to enjoying your life.







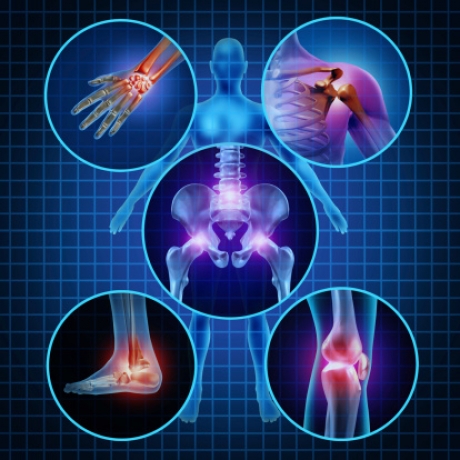

 Rotator cuff tendonitis occurs when the tendons and muscles that help move the shoulder joint are inflamed or irritated. This condition commonly occurs in people who play sports that frequently require extending the arm over the head, such as tennis, swimming and pitching. Most people with rotator cuff tendinitis can regain full function of the shoulder without any pain after treatment.
Rotator cuff tendonitis occurs when the tendons and muscles that help move the shoulder joint are inflamed or irritated. This condition commonly occurs in people who play sports that frequently require extending the arm over the head, such as tennis, swimming and pitching. Most people with rotator cuff tendinitis can regain full function of the shoulder without any pain after treatment.