November is American Diabetes Month, a time set aside to raise awareness about diabetes and its associated risk factors.
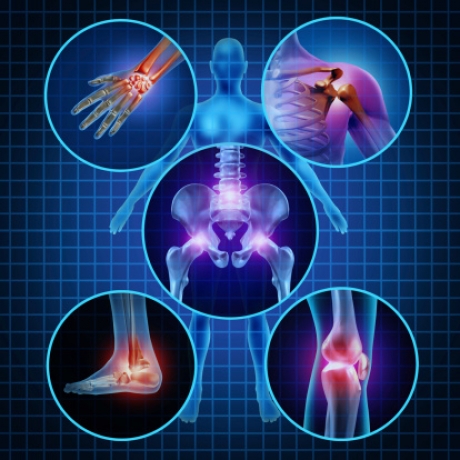
Did you know that if you are an individual living with diabetes, you are at higher risk for some bone and joint disorders?
Certain factors such as nerve damage (diabetic neuropathy), arterial disease and obesity may contribute to these conditions, but often the cause isn’t clear.
If you feel that you are experiencing any of these symptoms, talk with your endocrinologist or consult a board certified orthopedic physician who will take your medical history of diabetes into account when diagnosing your condition.
Charcot Joint
Charcot (shahr-HOK) joint, also called neuropathic arthropathy, occurs when a joint deteriorates because of nerve damage – a common complication of diabetes. Charcot joint primarily affects the feet.
Symptoms include numbness and tingling or loss of sensation in the affected joints. They may become unstable, swollen or deformed. If detected early, progression of the disease can be slowed. Limited weight bearing activities and use of orthotic supports to the affected joint and surrounding structures can help.
Diabetic Hand Syndrome
Diabetic hand syndrome, also called cheiroarthropathy, is a disorder in which the skin on the hands becomes waxy and thickened. Eventually finger movement is limited. What causes diabetic hand syndrome isn’t known but it is most common in people who have had diabetes for a long time.
Over time, individuals with diabetic hand syndrome become unable to fully extend their fingers or press their palms together flat. Better management of blood glucose levels and physical therapy can slow the progress of this condition.
Osteoporosis
Osteoporosis is a disorder that causes bones to become weak and prone to fracture. People who have type 1 diabetes have an increased risk of osteoporosis.
Osteoporosis rarely causes symptoms in the early stages. Eventually, when the disease is more advanced, individuals can experience loss of height, stopped posture or bone fractures. A healthy lifestyle, including weight bearing exercise such as walking, and eating a well-balanced diet rich in calcium and vitamin D – including supplements if needed – are the best ways to address this condition.
Osteoarthritis
Osteoarthritis is a joint disorder characterized by the breakdown of joint cartilage. It may affect any joint in the body. People who have type 2 diabetes have an increased risk of osteoarthritis, likely due to obesity – a risk factor for type 2 diabetes – rather than to the diabetes itself.
Osteoarthritis may cause joint pain, swelling and stiffness as well as loss of joint flexibility or movement. Treatment involves exercising and maintaining a healthy weight, caring for and resting the affected joint, pain medication and, in some cases, surgery. Complimentary treatment such as acupuncture and massage can be helpful.
DISH
Diffuse idiopathic skeletal hyperostosis (DISH), also called Forestier disease, is a hardening of tendons and ligaments that commonly affects the spine. DISH may be associated with type 2 diabetes, perhaps due to insulin or insulin-like growth factors that promote new bone growth.
Affected individuals may experience pain, stiffness or decreased range of motion in any affected part of the body. Treatment involves managing symptoms, usually with pain medication, and in rare cases may require surgery to remove bone that has grown due to the condition.
Dupuytren Contracture
Dupuytren contracture is a deformity in which one or more fingers are bent toward the palm. It’s caused by thickening and scarring of connective tissue in the palm of the hand and in the fingers. This condition is common in people who have had diabetes for a long time.
People affected by dupuytren contracture may notice thickening of the skin on the palm of their hand. Eventually, they may not be able to fully straighten one or more fingers. Steroid injections may help reduce inflammation. Surgery, injections and a minimally invasive procedure called aponeurotomy to break apart the thick tissue are other options if the condition prevents the ability to grasp objects.
Frozen Shoulder
Frozen shoulder is a condition characterized by shoulder pain and limited range of motion. It typically affects only one shoulder. Although the cause is unknown, diabetes is a common risk factor.
Frozen shoulder causes pain or tenderness with shoulder movement, stiffness of the joint and decreased range of motion. If started early, aggressive physical therapy can help preserve movement and range of motion in the joint.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is caused by a constriction of the hand’s central nerve by a ligament that runs across the palm. Diabetes may account for between 5 and 16 percent of all cases of carpal tunnel syndrome. The link between diabetes and carpal tunnel syndrome may be that the ligament becomes thickened in response to collagen glycation so that it presses on the nerve. Another possibility is that diabetic neuropathy – nerve disease – damages the nerves in the hand, making them more susceptible to carpal tunnel syndrome.
Strengthening and stretching exercises under the direction of a physical therapist may be helpful. Steroids and a wrist splint can be an interim measure, and surgery may be needed eventually.