If your New Year’s resolution is to commit to a triathlon in 2017, you’re probably in the early weeks of training for a spring or summer event. Training for a triathlon is tough but that’s part of the challenge – and the fun.
Before you get too far into your training, consider this; Four out of five amateur triathletes are injured while training, and three of those four are injured badly enough to be sidelined from their daily activities as well as their tri training.
The complexity of the sport and the broad range of knowledge needed to train and compete safely are contributing factors. The triathlete must learn about appropriate equipment, proper body mechanics, nutrition and hydration, injury prevention and overall training programs that prepare the body for the stresses of a triathlon.
Cross training for three events – running, biking and swimming – also increases the risk of certain overuse injuries, and an untreated injury in one part of the body can lead to problems elsewhere. For example, a knee injury from running can cause extra stress on the back, leading to lower back pain when cycling; and the cumulative effect of swimming and cycling can fatigue calf muscles, making legs more susceptible to injury during a run. Improper training can be a vicious cycle, resulting in injury and, ultimately, derailing your resolution to compete in a triathlon.
The good news is, most non-traumatic injuries are related to training errors that can be corrected – and an orthopedic physician with specialized knowledge in sports medicine and injury prevention can help.
Train Smart
The best way to avoid traumatic injury is to undertake a training program that balances strength, flexibility and endurance through weight lifting, stretching and cross training. But training techniques are not one size fits all. Each individual has a unique combination of anatomy, strength, endurance and flexibility, so what works well for one athlete isn’t always the best route for another.
Understanding the relationships between musculoskeletal groups related to swimming, cycling and running is key to triathlon training. An orthopedic surgeon can evaluate your physical conditioning, analyze your training techniques and correct errors that can lead to potential injuries, as well as provide important input into a training program optimized for your needs.
Heal Smart
The best training program can’t prevent all injuries. When injuries do occur, there are three things you need to know:
- How to evaluate the severity of the injury
- How to treat an overuse injury
- When to seek professional help
Congratulations for taking on a triathlon challenge. Whether you’re a first-time athlete or a seasoned tri gal or tri guy, training for and participating in the sport of triathlon involves a huge, months-long commitment. Unfortunately, sometimes things don’t go as planned and injury can overturn even the most dedicated competitor with the most detailed training plan.
When the unforeseen occurs, it is always best to seek medical evaluation from an experienced orthopedic physician. Often, if these issues are addressed early on, they can be treated without significant time loss from training and without surgery. An experienced orthopedic physician understands the sports medicine needs of patients and can be an important part of your team, helping you return to sport as soon as possible.
Preparing For A Triathlon
Make a plan:
- Select a competition that’s right for you
- Start your training gradually, begin with short distances and work up to longer distance, faster times and greater intensity
- Consider recruiting a training buddy to help keep you on track with your goals
- Check out websites such as USA Triathlon to locate training groups or routes in your area
Eat Properly
- Consume foods rich in nutritional content and high in complex carbs
- Increase your intake closer to race time, and supplement with energy gels and sports drinks as needed
Choose Proper Equipment
- Research water temps to see if you need a wetsuit
- Make sure your bike chains and pedals are working properly, and don’t forget your helmet
- Wear comfortable training shoes and avoid sporting a new pair that may lead to blisters
- If you experience severe or persistent pain while training, seek advice from an orthopedic physician before a more serious injury can occur


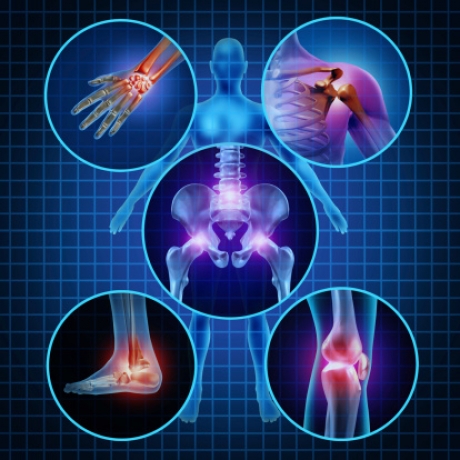

 Rotator cuff tendonitis occurs when the tendons and muscles that help move the shoulder joint are inflamed or irritated. This condition commonly occurs in people who play sports that frequently require extending the arm over the head, such as tennis, swimming and pitching. Most people with rotator cuff tendinitis can regain full function of the shoulder without any pain after treatment.
Rotator cuff tendonitis occurs when the tendons and muscles that help move the shoulder joint are inflamed or irritated. This condition commonly occurs in people who play sports that frequently require extending the arm over the head, such as tennis, swimming and pitching. Most people with rotator cuff tendinitis can regain full function of the shoulder without any pain after treatment.



